Micro-organisms
Micro-organisms by their very nature are opportunistic, exploiting chances to colonise or enter the body, which may result in infection. Health care associated infections (HCAIs) may be caused by a large number of different micro-organisms, a significant proportion of which are avoidable if sustainable and robust systems are in place to manage risks associated with infection.
We all have a professional and ethical responsibility to ensure our knowledge and skills are up-to-date and that we practice safely and competently at all times.
Infection or disease may be caused by different groups of micro-organisms such as bacteria, fungi, viruses or prions and these can result in a wide variety of infections. Not all infections are transmissible, however some, such as clostridium difficile (C. difficile), influenza and norovirus, have the potential to spread from one patient to another causing infection with additional significant implications for health and social care facilities.
Understanding how infections occur and how different micro-organisms act and spread is crucial to preventing infections.
Risk of infection
Infection can occur when micro-organisms are transferred from one patient to another, from equipment or the environment to patients or between staff.
Situations that pose the greatest risks include, but are not limited to:
By applying standard precautions at all times and to all patients, best practice becomes second nature and the risks of infection are minimised.
Hand hygiene
Preventing infections requires sustained compliance with a number of good practice areas - including the provision of clean environment, aseptic techniques, and the management of invasive devices. However, evidence shows that improving hand hygiene contributes significantly to the reduction of HCAIs.
Hand hygiene can be undertaken using soap and water or with hand sanitisers, namely alcohol hand gels.
Alcohol hand gels provide an efficient and effective way of disinfecting hands. However, alcohol is not a cleaning agent and hands that are visibly dirty or potentially contaminated must be washed with soap and water and dried thoroughly to remove dirt, viruses or spores.
Although it is not possible to 'sterilise' hands completely, the number of bacteria present can be reduced significantly through good hand hygiene practice.
Hand drying and conditioning
Wet hands transfer micro-organisms more effectively than dry ones, and inadequately dried hands can also be prone to developing skin damage. Disposable paper hand towels should be used to ensure hands are dried thoroughly. Disposable hand towels are placed in wall-mounted dispensers close to hand washing facilities.
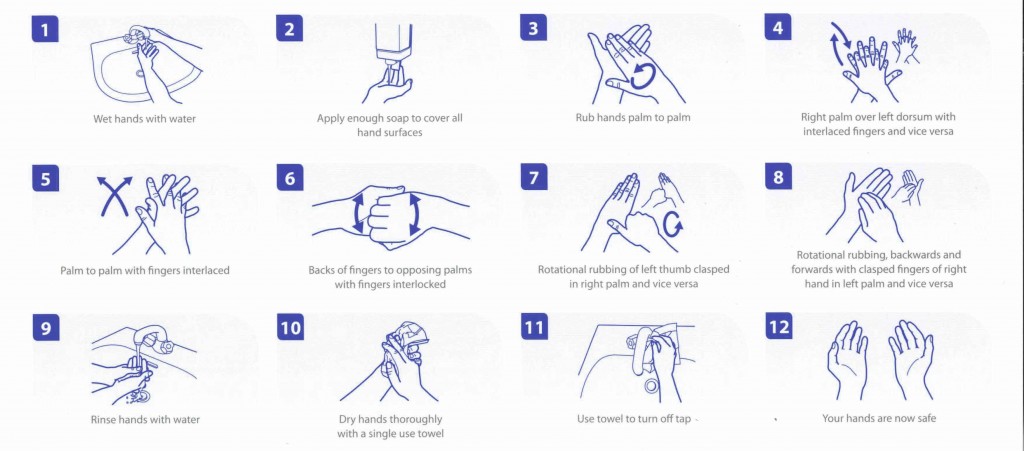
Hand Washing Technique
Using personal protective equipment
Personal protective equipment (PPE) is used to protect both health care workers and patients from risks of infection. The risk of infection occurring is reduced by preventing the transmission of micro-organisms to the patient via the hands of staff or vice versa. Gloves may also be required for contact with hazardous chemicals and some pharmaceuticals, for example; disinfectants or cytotoxic drugs. PPE includes items such as gloves, aprons, masks, goggles or visors.
Disposable gloves
Wearing gloves only when required is important, as the incorrect use of gloves can lead to several problems including:
Gloves should be worn whenever contact with blood and body fluids, mucous membranes or non-intact skin may occur, but should not be considered a substitute for hand hygiene. Hand hygiene must always be performed following the removal of gloves. Gloves should be put on immediately before the task is to be performed, then removed and discarded as soon as that procedure is completed. Gloves should never be worn 'just in case' as part of routine care.
The Control of Substances Hazardous to Health Regulations (2002) require employers to assess any substances hazardous to health, including biohazards within blood and body fluids (such as blood-borne viruses) and take steps to reduce the risk of exposure. Where exposure cannot be avoided, as is the case with a number of health care related activities, personal protective equipment, including gloves should be used.
Gloves can also present risks to the patient and health care worker. The choice of glove should be made following a risk assessment of the task about to be undertaken, the suitability of the gloves (including fit, comfort and dexterity) and any risks to the patient or to the health care worker.
Disposable plastics aprons
Disposable plastic aprons provide a physical barrier between clothing/skin and prevent contamination and wetting of clothing/uniforms during bathing/washing or equipment cleaning.
Aprons should be worn whenever there is a risk of contamination of uniforms or clothing with blood and body fluids and when a patient has a known or suspected infection. As with gloves, aprons should be changed as soon as the intended individual task is completed. Aprons should not be worn routinely during shifts as part of normal activity but should be reserved for when required. Aprons should be disposed of immediately after use in accordance with local waste policies.
Impervious (i.e. waterproof) gowns should be used when there is a risk of extensive contamination of blood or body fluids or when local policy dictates their use for certain settings.
Masks, visors and eye protection
Masks, visors and eye protection should be worn when a procedure is likely to result in blood and body fluids or substances splashing into the eyes, face or mouth.
Safe handling and disposal of waste
All health care and support staff should be educated in the safe handling of waste, including segregation, disposal and dealing with spillages.
Bags that are used for waste disposal have a colour coding which will be specific to the type of waste:

All waste must be disposed of in the correct bag and/or bin.
Spillage management
Spillages of blood and bodily fluids should be dealt with quickly, following your workplace's written policy for dealing with spillages.
The policy should include details of the chemicals staff should use to ensure that any spillage is disinfected properly, taking into account the surface where the incident happened.
Cleaning of the environment
Cleaning removes contaminants, including dust and soil, large numbers of microorganisms, and the organic matter that may shield them - for example, biofilms, faeces, blood and other bodily fluids. Cleanliness applies to the inanimate environment as well as equipment and fixtures and fittings.
The following principles are important for ensuring a clean and safe care environment is maintained:
Disinfection
This process uses chemical agents or heat to reduce the number of viable organisms. It may not necessarily inactivate all viruses and bacterial spores. Where equipment will tolerate sterilisation, disinfection should not be used as a substitute. The use of disinfectants is governed by the Control of Substances Hazardous to Health (COSHH) regulations which ensure that employers must assess and manage the risks from exposure to disinfectants and provide staff with information, instruction and training.
Decontamination of equipment
Decontamination is a combination of processes - cleaning, disinfection and/or sterilisation - that are used to ensure a reusable medical device or patient equipment is safe for further use. Equipment used in health care may be designated as single use, single patient use or reusable multi-patient use. Any equipment not designated as a single use item must be made safe following use to prevent micro-organisms being transferred from equipment to patients and potentially resulting in infection. Decontamination is the method for achieving this.
Cleaning is the critical element of the process and should always be undertaken thoroughly regardless of the level of decontamination required.
Single use equipment
Single use equipment (where the item can only be used once) should not be re-processed or re-used. Examples include disposable jugs, thermometer covers, syringes and needles.
Safe handling and disposal of sharps
Sharps include needles, scalpels, stitch cutters, glass ampoules, bone fragments and any sharp instrument. The main hazards of a sharps injury are blood borne viruses such as hepatitis B, hepatitis C and HIV.
It is not uncommon for staff to be injured by the unsafe or poor practice of others; for example, cleaners who sustain injuries as a result of sharps being placed in waste bins.
Sharps injuries are preventable and learning following incidents should be put in place to avoid repeat accidents.
To reduce the risk of injury and exposure to blood borne viruses, it is vital that sharps are used safely and disposed of carefully, following your workplace's agreed policies on use of sharps.
Legislation and sharps injuries
The overarching law is the Health and Safety at Work Act (1974) which places general duties on employers to ensure, so far as reasonably practicable, the health, safety and welfare of his or her employees.
Consequences of not complying with the law
Health care organisations can be subject to criminal law enforcement action if they fail to comply with the requirements of the law in relation to the prevention of sharps injuries.
In 2010 a hospital trust was fined more than �20,000 after a health care worker contracted hepatitis C following a sharps injury. The trust was found guilty of breaching the Health and Safety at Work Act (1974) and the Control of Substances Hazardous to Health Regulations (2002).
Sharps best practice points
You should ensure that:
If you notice any of the above procedures are not being followed properly by colleagues you should inform a senior member of staff immediately.
Managing the risk of Hepatitis B (HBV) and C (HCV)
Hepatitis B (HBV)
Because the virus is more infectious and has greater prevalence, the risk of contracting HBV from a sharps injury in a health care setting is much higher than HIV.
All nurses and health care assistants should be vaccinated against hepatitis B.
Hepatitis C (HCV)
There is currently no vaccine available that can prevent infection following exposure to the hepatitis C virus. Prevention is the key to avoiding exposure and subsequent infection, and staff should ensure they comply with local blood borne diseases policy and wear appropriate protective clothing, reporting any exposure incidents as these occur.